Oral Surgery Procedures
Cincinnati, OH
Two Locations to Serve You
State-of-the-Art Equipment
Low-Stress Setting
Request Appointment
Hero Request Form
Thank you for contacting us.
We will get back to you as soon as possible.
Please try again later.
Comprehensive Oral Surgery Procedures in Cincinnati
At Oral & Maxillofacial Surgery of Ohio, we understand that oral health is an essential aspect of your overall well-being. With two locations in Cincinnati, our practice is dedicated to providing comprehensive oral surgery procedures tailored to your specific needs. Whether you're dealing with wisdom teeth, require dental implants, or need facial trauma care, we're here to offer the highest standard of service in a professional, low-stress setting. Contact us today to schedule your consultation and take the first step toward optimal oral health. Contact us today to schedule an appointment.
- Dental implants: Restore missing teeth with durable, natural-looking replacements
- Bone grafting: Strengthen jawbone for future implants or other procedures
- Wisdom teeth: Remove impacted or problematic wisdom teeth
- Orthognathic surgery: Correct jaw alignment issues
- Facial trauma: Repair injuries to the face and jaw
- Tooth extractions: Remove damaged or decayed teeth
- Pre-prosthetic surgery: Prepare mouth for dentures or other prosthetics
- Oral pathology: Diagnose and treat oral diseases
- Exposure to impacted teeth: Manage complications from tooth removal
- 3D imaging: Utilize advanced imaging for precise treatment planning
- Anesthesia: Ensure comfort and safety during procedures
Dental Implants
What Are Dental Implants?
A natural tooth consists of a root and a crown. If you compare natural teeth to implant-supported replacement teeth, you’ll see they have the same basic parts. Both have a crown (the visible part used to chew food). Both have a root that holds the tooth securely under the gum and is anchored into the jaw. The difference is that the implant is made of titanium—the same time-tested material used by surgeons for artificial joints. When you lose a tooth, you lose both the root and the crown. To replace the tooth, the surgeon first replaces the root with a small dental implant.
Time is allowed for bone to heal and grow around the dental implant. The bone bonds with the titanium, creating a strong foundation for artificial teeth. A support post (abutment) is then placed on the implant, and a new replacement tooth (crown) is placed on top of the abutment. In many cases, a temporary replacement tooth can be attached to the implant immediately after it is placed. If all of your teeth are missing, a variety of treatment options are available to support the replacement teeth.
Surgical Advances in Dental Implants
Using the most recent advances in dental implant technology, Dr. Emami is able to place single-stage implants. These implants do not require a second procedure to uncover them but do require a minimum of six weeks of healing time before artificial teeth are placed. There are even situations where the implant can be placed at the same time as the tooth extraction—further minimizing your number of surgical procedures.
Dental implant placement is a team effort between an oral and maxillofacial surgeon and a restorative dentist. Dr. Emami performs the actual implant surgery, initial tooth extractions, and bone grafting if necessary. The restorative dentist (your dentist) fits and makes the permanent prosthesis. Your dentist will also make any temporary prosthesis needed during the implant process.
The Dental Implant Surgical Procedure
The procedure to place a dental implant takes 30 to 60 minutes for one implant and only two to three hours for multiple implants. The number of appointments and time required vary from patient to patient. The surgeon will bring great precision and attention to the details of your case.
Prior to surgery, you may receive antibiotics and for greater comfort, intravenous sedation or nitrous oxide (laughing gas). These options are discussed with you at your consultation appointment. A local anesthetic will be administered to numb the area where the dental implant will be placed.
When you are comfortable, the surgeon makes a small incision in the gum tissue to reveal the bone, creates space using special instruments, and gently inserts the titanium implant. The top of this implant is often visible through the gum. Sometimes it is better in the early stages of healing to have the implant covered by the gum tissue.
A good candidate is anyone missing one or more teeth or who is unhappy with their dentures. Age is not a factor. However, smoking, diseases such as diabetes, and radiation therapy to the area have been shown to lower the success rate of implant placement. X-rays of your jaw will be taken to evaluate whether they will accommodate implants. Detailed X-rays may also be required to determine if other tests or procedures are needed to place implants properly.
You may also need bone grafting if the sinus cavities in your upper jaw are very large, or very low, and extend into the tooth-bearing areas. This often occurs when teeth in the back of a person’s upper jaw have been removed many years before, and the amount of bone available for implant placement is limited. A “sinus grafting procedure” is then required. Most often, it is performed in the office with local anesthesia and perhaps sedation. During this procedure, the membrane that lines the sinus will be located and elevated. Bone will then be added to restore the bone height and ensure that dental implants of an adequate length can be placed. This procedure often can be performed at the time of implant placement.
Replacing Missing Teeth
Your teeth affect your whole body. When they’re healthy, you’re healthier too. A missing tooth can affect your bite, speech, and eating choices. As you rely more on your remaining teeth, you increase the chance they will wear out prematurely, or be damaged or lost. You may also experience headaches and/or jaw pain.
Who would want their appearance and health to deteriorate? That’s the natural consequence of missing teeth—the jaw literally melts away. Generally, people will lose 25% of their supporting jawbone structure within the first year after tooth loss. Dental implants are more easily placed when teeth are first extracted because bone replacement becomes more complex as time passes. The great news? Implants act just like your natural teeth. They safeguard and preserve your bone structure, oral health, and appearance. Your dentist and the implant surgeon will provide you with options so that you can make the most informed decision concerning tooth replacement.
Tooth Replacement Options
You can select from a number of different options to replace your missing teeth—from temporary to long-lasting solutions.
A good candidate is anyone missing one or more teeth, or who is unhappy with their dentures. Age is not a factor. However, smoking, diseases such as diabetes, and radiation therapy to the area have been shown to lower the success rate of implant placement. X-rays of your jaw will be taken to evaluate whether they will accommodate implants. Detailed X-rays may also be required to determine if other tests or procedures are needed to place implants properly.
Overview of Implant Placement
The Dental Implant Surgical Procedure
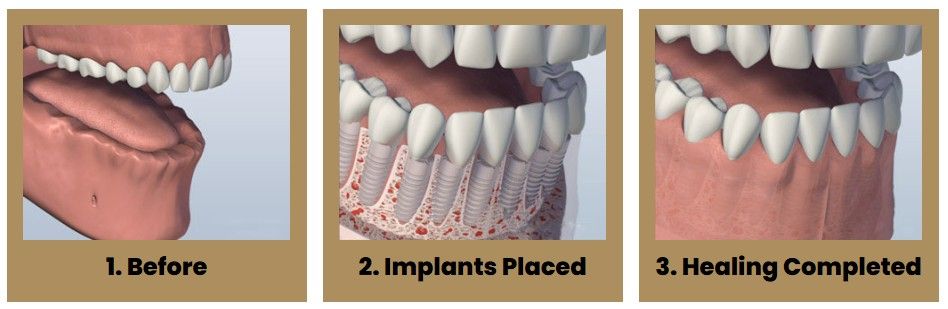
The procedure to place a dental implant takes 30 to 60 minutes for one implant and only two to three hours for multiple implants. The number of appointments and time required vary from patient to patient. The surgeon will bring great precision and attention to the details of your case.
Prior to surgery, you may receive antibiotics and for greater comfort, intravenous sedation or nitrous oxide (laughing gas). These options are discussed with you at your consultation appointment. A local anesthetic will be administered to numb the area where the dental implant will be placed.
When you are comfortable, the surgeon makes a small incision in the gum tissue to reveal the bone, creates space using special instruments, and gently inserts the titanium implant. The top of this implant is often visible through the gum. Sometimes it is better in the early stages of healing to have the implant covered by the gum tissue.
A good candidate is anyone missing one or more teeth or who is unhappy with their dentures. Age is not a factor. However, smoking, diseases such as diabetes, and radiation therapy to the area have been shown to lower the success rate of implant placement. X-rays of your jaw will be taken to evaluate whether they will accommodate implants. Detailed X-rays may also be required to determine if other tests or procedures are needed to place implants properly.

Healing after Dental Implant Surgery
Now the healing begins. The length of time varies from person to person, depending upon the quality and quantity of bone. In some cases, implants may be restored immediately after they are placed. The surgeon will advise you on follow-up care and timing. After the initial phase of healing, the surgeon places an abutment (support post) or a healing cap onto the dental implant during a brief follow-up visit. This allows gum tissue to mature and provides access to the implant.
Occasionally, impressions are made at the time the implant is placed. This enables the crown to be ready when the implants have healed. How long your mouth needs to heal is determined by a variety of factors. Follow-up care (one to four appointments) is usually needed to ensure that your mouth is healing well and to determine when you are ready for the restorative phase of your treatment.
It may be beneficial to perform a soft tissue graft to obtain stronger, more easily cleaned and natural appearing gum tissue in the area around the implant. This process involves moving a small amount of gum tissue from one part of your mouth to the area around the implant. Most often, it is a brief and relatively comfortable procedure.
Whether it’s one tooth or all of your teeth that are being replaced, your dentist will complete the restoration by fitting the replacement tooth (crown) to the dental implant.
When are dental implants placed?
Implants are often placed several months after extraction. At times, an implant may be placed immediately after extraction of a tooth. This may involve a little more risk, but it simplifies the process—you won’t have to wait for another appointment to place the implant. When infection or other problems with the bone are present, immediate implant placement is not the best treatment.
If your tooth has been missing for some time, the adjacent support bone is likely to grow thinner and shrink. This occurs because the root of the natural tooth has to be present to stimulate the bone. As much as one-third of your jaw’s thickness can be lost in the year following tooth extraction. If you are missing enough bone, you may benefit from having additional bone grafted into the area. This ensures the that implant will be adequately supported when it is placed in the jaw.
How many implants do I need?
Most frequently, one implant per missing tooth is placed. Because many of the larger teeth in the back of your jaws have two or three roots, the most common approach is to replace missing back teeth with larger implants.
Missing All Upper or Lower Teeth
Missing All Lower Teeth
Although many patients have no problem wearing an upper denture, some people find it difficult to wear and eat with lower dentures. Several implant-supported replacement options are available if you are missing all of your lower teeth.
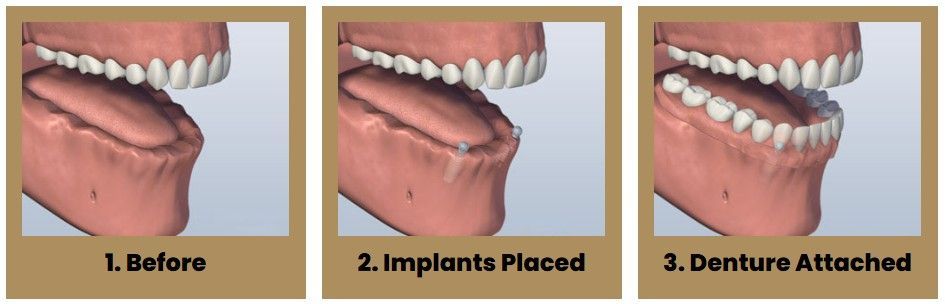
Ball Attachment Denture
One option is to have two implants placed in your lower jaw and a denture made that snaps onto these implants. This option allows your lower denture to be more stable while chewing than without implants. However, there will still be movement of your lower denture, and sore spots will occur if any food particles, especially seeds, are caught under it. As with all removable replacement teeth, you still will need periodic appointments for denture adjustment.
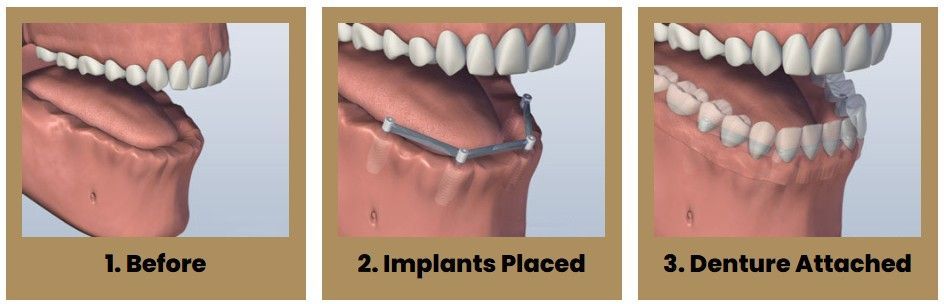
Bar Attachment Denture
Another option involves placing four to six implants, depending on your jaw size or shape, into your lower jaw. After healing is complete, the implants are connected with a custom-made support bar. Your denture will be made with special internal retention clips that attach onto the support bar, enabling the denture to snap firmly into place. This is called an “overdenture.” The advantage of this option is that it is much more stable than the first option and allows very little denture movement. Your denture is still removable for easy cleaning and maintenance.
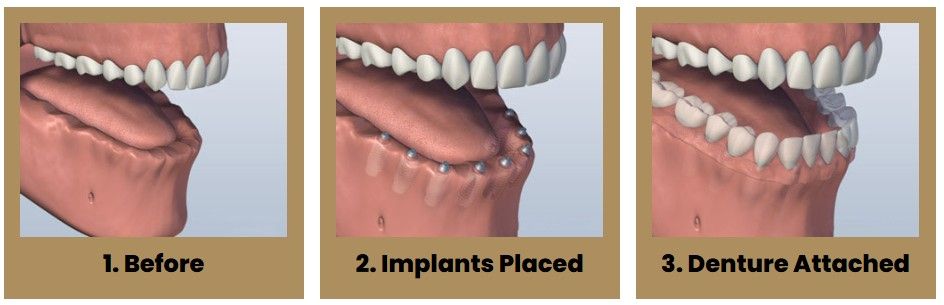
Screw Retained Denture
A third option involves placing five or more implants in your jaw and attaching a permanent denture. Your denture is held in place by screws or clasps that secure it to the support posts or bar. It doesn’t touch the gum tissue, which allows you to clean under the denture without removing it. This denture will replace all of your missing lower teeth and will not be removed except at maintenance visits. Although cleaning under your denture without removing it is more time-consuming and requires more dexterity, many patients who want a permanent denture prefer this option.
Individual Implants
The final option is to have all of your teeth individually replaced so that they will appear to be growing out of your gum tissue and will most closely resemble the appearance of your natural teeth. This option usually requires eight or more implants. Separate abutments or support posts for each one of these implants will be made, and crowns for each missing tooth will be placed. The teeth are often joined together for sinus grafting to replace bone height strength and support. Overall, this is the most costly option, because it requires the most implants and individual replacement tooth fabrication. Your replacement options may also be limited by the current size and shape of your jawbone.
What if I’m missing all of my upper teeth?
A similar range of treatment options is also available for your upper jaw. However, because the bone is not as hard as that in the lower jaw, people often need more implants to support their new replacement teeth. Depending upon the number of implants to be placed, it may be possible to eliminate the need for covering the roof of your mouth with a complete denture. This option allows you to fully taste your food and gives you a better sense of its temperature. Your denture will feel more natural. You will still have a removable denture, which makes cleaning the support bar and denture much easier
Implant Retained Upper Denture
Depending upon the number of implants to be placed, it may be possible to eliminate the need for covering the roof of your mouth with a complete denture. This option allows you to fully taste your food and gives you a better sense of its temperature. Your denture will feel more natural. You will still have a removable denture, which makes cleaning the support bar and denture much easier.
Individual Upper Implants
If you want a restoration that is similar to your natural teeth and therefore not removable, you probably will need eight to ten individual implants placed. This is followed after healing by the placement of the abutments and new replacement crowns.
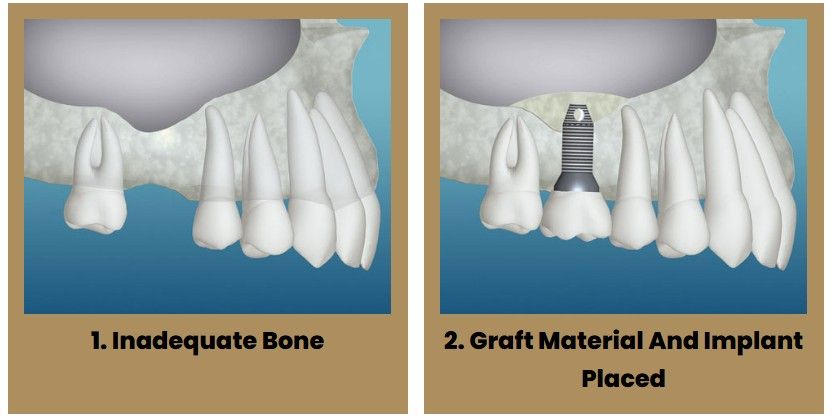
Bone Grafting for Implants
Do I have enough bone for dental implants?
Although many patients have no problem wearing an upper denture, some people find it difficult to wear and eat with lower dentures. Several implant-supported replacement options are available if you are missing all of your lower teeth.
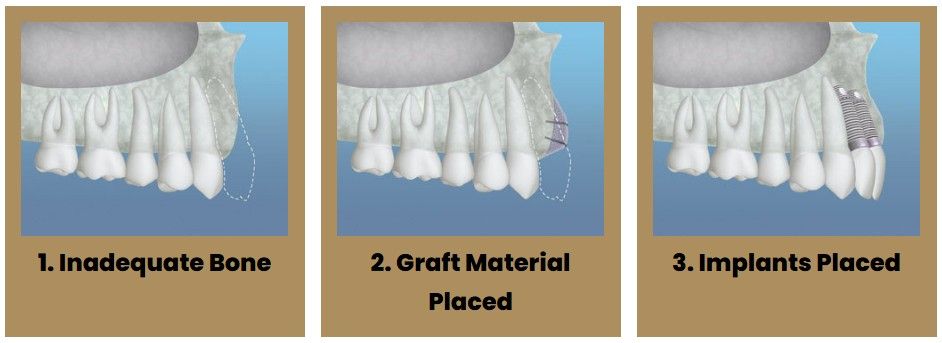
There may be inadequate bone for implant placement if your tooth was removed many years ago, and your bony ridge is extremely thin. In this case, a bone graft can be placed next to the thin bone and allowed to heal for up to six months. After the graft has fused to your pre-existing bone, the ridge will be re-entered and the implant placed. Bone grafting is usually a relatively comfortable office procedure. Many different bone-grafting materials are available, including your own bone.
You may also need bone grafting if the sinus cavities in your upper jaw are very large, or very low, and extend into the tooth-bearing areas. This often occurs when teeth in the back of a person’s upper jaw have been removed many years before, and the amount of bone available for implant placement is limited. A “sinus grafting procedure” is then required. Most often, it is performed in the office with local anesthesia and perhaps sedation. During this procedure, the membrane that lines the sinus will be located and elevated. Bone will then be added to restore the bone height and ensure that dental implants of an adequate length can be placed. This procedure often can be performed at the time of implant placement.
Implant Supported Overdenture
An Implant Supported Overdenture is a contemporary restoration that has revolutionized the way surgeons and dentists think of replacing a full set of teeth. Standard dentures are unsecured prostheses with inherent limitations. Most often, dentures are painful, inconvenient, and unstable. Such dentures can make chewing foods difficult, limiting the foods that you once enjoyed. Modern dentistry can help with implant-supported dentures.
The Implant Supported Overdenture treatment concept replaces your missing teeth with a full dental bridge supported by dental implants. Fewer implants are needed, and overall treatment time and cost is reduced. An Implant Supported Overdenture solution also ensures greater stability in the bone, reducing the need for bone graft surgery to increase bone volume. Implant-supported overdentures stay connected with bar and clip attachment methods or use a variety of abutment-based attachments (ball, magnets, and resilient stud attachments such as Locators). The most appropriate attachment system for your individual needs relates to a variety of factors that is determined early in the treatment. Typically, a temporary set of teeth can be placed on the same day of surgery. The temporary teeth allow you to lead a normal life immediately after surgery. After a short healing period, your dentist will place the final bridge. Your quality of life is improved, and you can start enjoying your favorite foods again with renewed confidence.
Implant Supported Overdentures offer you many advantages:
- A cost-effective solution. When compared to some other implant supported restoration methods, your new replacement teeth require fewer implants for each jaw. With fewer implants required, the cost is lowered.
- Reduced need for bone grafting. The special angled placement of two of the implants ensures a secure and stable anchorage for the replaced arch, often making bone grafting unnecessary.
- Faster treatment and healing time. Your replacement arch can be attached to your implants immediately after insertion.
Scientifically proven and documented. Implant Supported Overdentures have had good clinical outcomes from decade long studies with favorable results.
After Implant Placement FAQ
What can I use for teeth while the implants heal?
Many options are available, and they are tailored to your specific requirements. If you need a replacement tooth while the implants are healing, temporary removable teeth or a temporary bridge can be made. If all of your teeth are missing, we can usually modify your present complete denture or make you a new temporary denture. If you would prefer non-removable teeth during the healing phase, temporary transitional implants usually can be placed along with the permanent implants, and temporary teeth may be made and inserted the same day. Depending on your particular situation, some implants can be placed and “loaded” immediately. This means a temporary or permanent replacement tooth can be placed on, or shortly after, the day the implant is placed.
What are the potential problems after dental implant surgery?
Although it is natural to be concerned about the pain that may be caused by these procedures, most patients do not experience severe or significant post-operative pain. Pain medication and antibiotics will be prescribed for you to make your recovery as easy as possible. Occasionally, some people develop post-operative infections that require additional antibiotic treatment. Even though great care is taken to place the implant precisely, occasionally adjacent teeth are injured in the placement process. In addition, there is a chance that the nerve in the lower jaw, which provides sensation to your lower lip and chin, may be affected. If you are missing quite a lot of bone, it might be difficult to place an implant without infringing on the nerve space. Although we take great care to avoid this nerve, occasionally it is irritated during the procedure, resulting in tingling, numbness, or a complete lack of sensation in your lip, chin, or tongue. Usually these altered sensations will resolve within time, but they can be permanent and/or painful. If you notify us of post-operative numbness as soon as possible, it will allow us to manage your care in the most appropriate way.
How long will the implants last?
Implants usually last a long time. When patients are missing all of their teeth, long-term studies (more than 30 years) show an 80 to 90 percent success rate. For patients missing one or several teeth, recent studies show a success rate of greater than 95 percent, which compares favorably with other areas in the body that receive implant replacement (such as hips or knees). However, if one of your dental implants either doesn’t heal properly or loosens after a period of time, you may need to have it removed. After the site heals (or on occasion at the time of removal), another implant usually can be placed.
When are the replacement teeth attached to the implant?
The replacement teeth are usually attached to the implant when adequate healing has occurred and your jaw bone is firmly fused to the implant. Depending on a variety of factors, it may be possible to begin this phase of your treatment immediately or shortly after implant placement. We will review the most appropriate treatment sequence and timing for your particular situation.
The dental work required to complete your treatment is complex. Most of the work involves actually making the new teeth before they are placed. Your appointments are considered more comfortable and more pleasant than previous methods of tooth replacement. Frequently, this process can be performed without local anesthesia.
Your restorative treatment begins with specialized impressions that allow us to produce a replica of your mouth and implants. We will also make “bite” records so that we see the relationship of your upper and lower jaws. With this information, we will make the abutments (support posts) that attach your replacement teeth to your implants. Various types of abutments exist. Frequently, we can use “off the shelf” abutments. Other times, custom abutments must be made of gold or a tooth-colored ceramic material. As you can imagine, these custom made abutments add to the cost and treatment time involved. Which abutment to use is a decision that often cannot be made until after healing is complete and impressions have been made.
The number of appointments and the amount of time required for each appointment is different for each patient. No two cases are exactly the same and regardless of the number of teeth replaced, the work must be completed with great precision and attention to detail. If you are having only a few teeth replaced, as few as three short appointments may be required. Between appointments, we will need time to complete the necessary lab work to make your replacement teeth. It is most beneficial that you keep all of your scheduled appointments.
If your final restoration is a removable denture, you will need to come to as many as five office appointments (although it may be fewer) over the following several months. During these appointments, we will perform a series of impressions, bites and adjustments in order to make your new teeth, as well as the custom support bars, snaps, magnets, or clips that will secure your teeth to the implants. During this period, every effort will be made to ensure you have comfortable, temporary replacement teeth.
In general, once your implants are placed, you can expect your tooth replacement treatment to be completed anywhere from 1 to 12 months. For these reasons, it is difficult for us to tell you exactly how much the restorative phase of your treatment will cost, although you should receive a reasonable estimate from our office. It also is difficult to give you a specific timeframe for completion of your treatment until after the implants are ready for restoration.
How do I clean my new teeth?
As with natural teeth, it is important that you clean implant-supported restorations regularly with toothbrushes, floss and any other recommended aids. You should also visit your dentist several times each year for hygiene and maintenance. As with regular dentures and other tooth replacements, your implants and their associated components are subject to wear and tear and eventually will need repair, including clip replacement, relines, screw tightening, and other adjustments.
Will one doctor do everything?
Usually, a dental surgeon places the implant(s) and performs other necessary surgical procedures—your general dentist provides the temporary and permanent replacement teeth. Both doctors are involved in planning your dental treatment. Also, depending upon a variety of factors, different dental specialists may help with your dental care.
How much does dental implant treatment cost?
Before treatment begins, every effort will be made to give you an accurate estimate of all the expenses involved in placing the implants and making your replacement teeth. In many cases, there is an initial charge for the diagnostic work-up, including study models, X-rays, and the fabrication of a surgical template to ensure the best possible result. In addition, you will be charged for the abutment or support post(s) plus the crown, dentures, or anything else that will be placed over the implants, including temporary restorations. Periodic maintenance, such as hygiene visits, tissue conditioners, denture relines, and other repairs, will also incur additional charges.
When different doctors are involved in your treatment, you will be charged separately for their services. We will try to assist you in estimating what your actual payments will be after we evaluate your insurance coverage or other third- party payments. Also, you should consider your personal financial investment in each treatment option, as some insurance companies provide limited or no coverage.
Each patient is unique, and it is not possible for us to discuss every option and every contingency for treatment outcome. This website is intended to help you understand the general treatment options available to you. If your specific treatment options are not clear, please contact us. We will be happy to answer any questions you have about your dental care.
Cost of Dental Implants
Considering the Cost of Dental Implants
Dental implants have been available for several decades. However, for most patients, they are still a relatively new concept. When considering the cost of dental implants and comparing quotes, there are several important points that should be kept in mind.
Longevity
When comparing the cost of dental implants to other tooth replacement methods, such as dentures and bridges, it is important to take into consideration the longevity offered by dental implants that is not always afforded by other, more traditional methods.
While dentures and bridges are initially less expensive, their affordability can be short-lived. Because these older methods require repair and replacement every five to 10 years, they are often more expensive over time. By contrast, dental implants, when properly placed and cared for, can last a lifetime.
Jaw Bone Health
Over time, when a tooth is missing, the jaw bone deteriorates. So while a denture or bridge may seem to function similarly to a tooth, underneath the surface damage is being done to the jaw bone and ultimately to the structure of the face. This can result in the distortion of the shape of a person’s face, leading to additional cosmetic costs down the road.
On the other hand, dental implants are made of titanium, which actually integrates with the jaw bone, strengthening it and stimulating bone growth. This preserves the natural strength and quality of the mouth, lessening problems in the future.
Quality of Life
Dental implants can be seen as a long-term investment not only in terms of money but also in terms of quality of life. A dental implant is the closest thing to a natural tooth. In addition to allowing the patient to eat the same healthy foods he or she has always enjoyed, it also eliminates the day-to-day hassles and possible embarrassment that are frequently caused by dentures.
Comparing Dental Implant Quotes
There are several steps (and often multiple professionals) involved in the placement of a dental implant. When comparing quotes, it’s important to factor in the cost of each of these steps:
- Exams/office visits
- Tooth/root extraction
- Bone grafting
- Placement of the titanium root (the “dental implant”)
- Placement of the crown
- X-rays, pre/post operative care
Financing for Dental Implants
First, check with your dental insurance carrier to see what portion, if any, of dental implants they cover. There are health care credit companies that offer no-interest and low-interest loans for medical procedures including dental implants.
Dental Implants are an investment in your health as well as your appearance. A full set of teeth makes eating a pleasure again, making it easier to eat a balanced, healthy diet. A full set of teeth also preserves the contours of the face, keeping you from looking old before your time.
Schedule Your Consultation
The only way to receive an accurate price quote is to call us and come in for a consultation, and we can give you a specific price for your case. Please call us at Jager Court at (513) 232-4600 or Banning Road at (513) 923-1500 to schedule your consultation.
Bone Grafting
Major & Minor Bone Grafting
Missing teeth over a period of time can cause your jaw bone to atrophy, or resorb. This often results in poor quality and quantity of bone suitable for the placement of dental implants as well as long-term shifting of remaining teeth and changes to facial structure. Most patients, in these situations, are not candidates for dental implants.
Fortunately, today we have the ability to grow bone where it is needed. This not only gives us the opportunity to place implants of proper length and width, but it also gives us a chance to restore functionality and aesthetic appearance.
Major Bone Grafting
Bone grafting can repair implant sites with inadequate bone structure due to previous extractions, gum disease, or injuries. The bone is either obtained from a tissue bank, or your own bone is taken from the jaw, hip, or tibia (below the knee). Sinus bone grafts are also performed to replace bone in the posterior upper jaw. In addition, special membranes may be utilized that dissolve under the gum to protect the bone graft as well as encourage bone regeneration. This is called guided bone regeneration, or guided tissue regeneration.
Major bone grafts are typically performed to repair defects of the jaws. These defects may arise as a result of traumatic injuries, tumor surgery, or congenital defects. Large defects are repaired using the patient’s own bone. This bone is harvested from a number of different areas depending on the size needed. The skull (cranium), hip (iliac crest), and lateral knee (tibia) are common donor sites. These procedures are routinely performed in an operating room and require a hospital stay.
Jaw Bone Health
When one or more teeth are missing, it can lead to bone loss at the site of the gap. This loss of jaw bone can develop into additional problems, both with your appearance and your overall health. You may experience pain, problems with your remaining teeth, altered facial appearance, and eventually even the inability to speak and/or eat normally.
In the same way that muscles are maintained through exercise, bone tissue is maintained by use. Natural teeth are embedded in the jaw bone and stimulate the jaw bone through activities such as chewing and biting. When teeth are missing, the alveolar bone, or the portion of the jaw bone that anchors the teeth into the mouth, no longer receives the necessary stimulation it needs and begins to break down, or resorb. The body no longer uses or “needs” the jaw bone, so it deteriorates.
Potential Consequences of Tooth and Jaw Bone Loss
- Problems with remaining teeth, including misalignment, drifting, loosening, and loss
- Collapsed facial profile
- Limited lip support
- Skin wrinkling around the mouth
- Distortion of other facial features
- Jaw (TMJ or temporomandibular joint) pain, facial pain, and headaches
- Difficulty speaking and communicating
- Inadequate nutrition as a result of the inability to chew properly and painlessly
- Sinus expansion
Jaw Bone Loss and Deterioration
Reasons for Jaw Bone Loss and Deterioration
The following are the most common causes for jaw bone deterioration and loss that may require a bone grafting procedure:
Tooth Extractions
When an adult tooth is removed and not replaced, jaw bone deterioration may occur. Natural teeth are embedded in the jaw bone and stimulate the jaw bone through activities such as chewing and biting. When teeth are missing, the alveolar bone, or the portion of the jaw bone that anchors the teeth in the mouth, no longer receives the necessary stimulation and begins to break down, or resorb. The body no longer uses or “needs” the jaw bone, so it deteriorates and goes away.
The rate at which the bone deteriorates, as well as the amount of bone loss that occurs, varies greatly among individuals. However, most loss occurs within the first 18 months following the extraction and will continue gradually throughout your life.
Periodontal Disease
Periodontal diseases are ongoing infections of the gums that gradually destroy the support of your natural teeth. Periodontal disease affects one or more of the periodontal tissues: alveolar bone, periodontal ligament, cementum, or gingiva. While there are many diseases that affect the tooth-supporting structures, plaque-induced inflammatory lesions make up the majority of periodontal issues and are divided into two categories: gingivitis and periodontitis. While gingivitis, the less serious of the diseases, may never progress into periodontitis, it always precedes periodontitis.
Dental plaque is the primary cause of gingivitis in genetically-susceptible individuals. Plaque is a sticky colorless film, composed primarily of food particles and various types of bacteria, that adheres to your teeth at and below the gum line. Plaque constantly forms on your teeth, even minutes after cleaning. Bacteria found in plaque produces toxins, or poisons, that irritate the gums. Gums may become inflamed, red, swollen, and bleed easily. If this irritation is prolonged, the gums will separate from the teeth causing pockets (spaces) to form. If daily brushing and flossing is neglected, plaque can harden into a rough, porous substance known as calculus (or tartar). This can occur both above and below the gum line.
Periodontitis is affected by bacteria that adheres to the tooth’s surface along with an overly aggressive immune response to these bacteria. If gingivitis progresses into periodontitis, the supporting gum tissue and bone that hold teeth in place deteriorates. The progressive loss of this bone, the alveolar, can lead to the loosening and subsequent loss of teeth.
Dentures/Bridgework
Unanchored dentures are placed on top of the gum line, but they do not provide any direct stimulation to the underlying alveolar bone. Over time, the lack of stimulation causes the bone to resorb and deteriorate. Because this type of denture relies on the bone to hold them in place, people often experience loosening of their dentures and problems eating and speaking. Eventually, bone loss may become so severe that dentures cannot be held in place with strong adhesives, and a new set of dentures may be required. Proper denture care, repair, and refitting are essential to maintaining oral health.
Some dentures are supported by anchors, which do help adequately stimulate, and therefore preserve bone. With bridgework, the teeth on either side of the appliance provide sufficient stimulation to the bone, but the portion of the bridge that spans the gap where the teeth are missing receives no direct stimulation. Bone loss can occur in this area.
By completing a bone graft procedure, Dr. Emami is now able to restore bone function and growth, thereby halting the effects of poor denture care.
Facial Trauma
When a tooth is knocked out or broken to the extent that no biting surface is left below the gum line, bone stimulation stops, which results in jaw bone loss. Some common forms of tooth and jaw trauma include: teeth knocked out from injury or accident, jaw fractures, or teeth with a history of trauma that may die and lead to bone loss years after the initial trauma.
A bone grafting procedure would be necessary to reverse the effects of bone deterioration, restoring function and promoting new bone growth in traumatized areas.
Misalignment
Misalignment issues can create a situation in the mouth where some teeth no longer have an opposing tooth structure. The unopposed tooth can over-erupt, causing deterioration of the underlying bone.
Issues such as TMJ problems, normal wear-and-tear, and lack of treatment can also create abnormal physical forces that interfere with the teeth’s ability to grind and chew properly. Over time, bone deterioration can occur where the bone is losing stimulation.
Osteomyelitis
Osteomyelitis is a type of bacterial infection in the bone and bone marrow of the jaw. This infection leads to inflammation, which can cause a reduction of blood supply to the bone. Treatment for osteomyelitis generally requires antibiotics and the removal of the affected bone. A bone graft procedure may be required to restore bone function and growth lost during removal.
Tumors
Benign facial tumors, though generally non-threatening, may grow large and require the removal of a portion of the jaw. Malignant mouth tumors almost always spread into the jaw, requiring the removal of the affected section of the jaw. In both cases, reconstructive bone grafting is usually required to help restore normal function to the jaw. Grafting in patients with malignant tumors may be more challenging because treatment of the cancerous tumor generally requires removal of the surrounding soft tissues as well.
Developmental Deformities
Some conditions or syndromes are characterized by missing portions of the teeth, facial bones, jaw, or skull. Drs. Emami may be able to perform a bone graft procedure to restore bone function and growth where it may be absent.
Sinus Deficiencies
When molars are removed from the upper jaw, air pressure from the air cavity in the maxilla (maxillary sinus) causes resorption of the bone that formerly helped keep the teeth in place. As a result, the sinuses become enlarged—a condition called hyperpneumatized sinus.
This condition usually develops over several years and may result in insufficient bone from the placement of dental implants. Drs. Emami can perform a procedure called a “sinus lift” that can treat enlarged sinuses.
About Bone Grafting
What is Bone Grafting?
Over a period of time, the jaw bone associated with missing teeth atrophies and is reabsorbed. This often leaves a condition in which there is poor quality and quantity of bone suitable for the placement of dental implants. In these situations, most patients are not candidates for the placement of dental implants.
With bone grafting, we now have the opportunity to not only replace bone where it is missing, but we also have the ability to promote new bone growth in that location. This not only gives us the opportunity to place implants of proper length and width, but it also gives us a chance to restore functionality and aesthetic appearance.
Types of Bone Grafts
Autogenous Bone Grafts
Autogenous bone grafts, also known as autografts, are made from your own bone, taken from somewhere else in the body. The bone is typically harvested from the chin, jaw, lower leg bone, hip, or the skull. Autogenous bone grafts are advantageous in that the graft material is your own live bone, meaning it contains living cellular elements that enhances bone growth, also eliminating the risk of your body rejecting the graft material since it comes from you.
However, one downside to the autograft is that it requires a second procedure to harvest bone from elsewhere in the body. Depending on your condition, a second procedure may not be recommended.
Allogenic Bone
Allogenic bone, or allograft, is dead bone harvested from a cadaver then processed using a freeze-dry method to extract the water via a vacuum. Unlike autogenous bone, allogenic bone cannot produce new bone on its own. Rather, it serves as a framework, or scaffold, over which bone from the surrounding bony walls can grow to fill the defect or void.
Xenogenic Bone
Xenogenic bone is derived from non-living bone of another species, usually a cow. The bone is processed at very high temperatures to avoid the potential for immune rejection and contamination. Like allogenic grafts, xenogenic grafts serve as a framework for bone from the surrounding area to grow and fill the void.
Both allogenic and xenogenic bone grafting have an advantage of not requiring a second procedure to harvest your own bone, as with autografts. However, because these options lack autograft’s bone-forming properties, bone regeneration may take longer than with autografts and have a less predictable outcome.
Bone Graft Substitutes
As a substitute to using real bone, many synthetic materials are available as safe and proven alternatives, including:
Demineralized Bone Matrix (DBM)/Demineralized Freeze-Dried Bone Allograft (DFDBA)
This product is processed allograft bone, containing collagen, proteins, and growth factors that are extracted from the allograft bone. It is available in the form of powder, putty, chips, or as a gel that can be injected through a syringe.
Graft Composites
Graft composites consist of other bone graft materials and growth factors to achieve the benefits of a variety of substances. Some combinations may include: collagen/ceramic composite, which closely resembles the composition of natural bone, DBM combined with bone marrow cells, which aid in the growth of new bone or a collagen/ceramic/autograft composite.
Bone Morphogenetic Proteins
Bone morphogenetic proteins (BMPs) are proteins naturally produced in the body that promote and regulate bone formation and healing.
Synthetic materials also have the advantage of not requiring a second procedure to harvest bone, reducing risk and pain. Each bone grafting option has its own risks and benefits. Dr. Emami will determine which type of bone graft material best suited to your particular needs.
Ridge Augmentation
What is a ridge augmentation?
A ridge augmentation is a common dental procedure often performed following a tooth extraction. This procedure helps recreate the natural contour of the gums and jaw that may have been lost due to bone loss from a tooth extraction or for another reason.
The alveolar ridge of the jaw is the bone that surrounds the roots of teeth. When a tooth is removed, an empty socket is left in the alveolar ridge bone. Usually, this empty socket will heal on its own, filling with bone and tissue. Sometimes when a tooth is removed, the bone surrounding the socket breaks and is unable to heal on its own. The previous height and width of the socket will continue to deteriorate.
Rebuilding the original height and width of the alveolar ridge is not always medically necessary but may be required for dental implant placement or for aesthetic purposes. Dental implants require bone to support their structure, and a ridge augmentation can help rebuild this bone to accommodate the implant.
How is a ridge augmentation accomplished?
A ridge augmentation is accomplished by placing bone graft material in the tooth socket. It is often done immediately after the tooth is removed to avoid the need for a second procedure later. Next, the gum tissue is placed over the socket and secured with sutures. Dr. Emami may choose to use a space-maintaining product over the top of the graft to facilitate new bone growth. Once the socket has healed, the alveolar ridge can be prepared for dental implant placement.
A ridge augmentation procedure is typically performed in Dr. Emami’s office under local anesthesia. Some patients may also request sedative medication.
Sinus Lift
What is a sinus lift?
The maxillary sinuses are behind your cheeks and on top of the upper teeth. These sinuses are empty, air-filled spaces. Some of the roots of the natural upper teeth extend up into the maxillary sinuses. When these upper teeth are removed, there is often just a thin wall of bone separating the maxillary sinus and the mouth. Dental implants need bone to hold them in place. When the sinus wall is very thin, it is impossible to place dental implants in this bone.
The key to a successful and long-lasting dental implant is the quality and quantity of jaw bone to which the implant will be attached. If bone loss has occurred due to injury or periodontal disease, a sinus augmentation can raise the sinus floor and allow for new bone formation. A sinus lift is one of the most common bone-grafting procedures for patients with bone loss in the upper jaw. The procedure seeks to grow bone in the floor of the maxillary sinus above the bony ridge of the gum line that anchors the teeth in the upper jaw. This enables dental implants to be placed and secured in the new bone growth.
Am I a candidate for a sinus lift procedure?
A sinus lift may be necessary if you:
- are missing more than one tooth in the back of your jaw
- are missing a significant amount of bone in the back of your jaw
- are missing teeth due to a birth defect or condition
- are missing most of the maxillary teeth and require support for dental implants
How is a sinus lift accomplished?
Most commonly, a small incision is made on the premolar or molar region to expose the jaw bone. A small opening is cut into the bone, and the membrane lining the sinus is pushed upward. The underlying space is filled with bone grafting material, either from your own body or from other sources. Sometimes, synthetic materials that imitate bone formation are used. After the bone is implanted, the incision is sutured, and the healing process begins. After several months of healing, the bone becomes part of the patient’s jaw, and dental implants can be inserted and stabilized in the newly formed sinus bone.
If enough bone between the upper jaw ridge and the bottom of the sinus is available to sufficiently stabilize the implant, sinus augmentations, and implant placement can sometimes be performed as a single procedure. If not enough bone is available, the sinus augmentation will have to be performed first, then the graft will have to mature for up to several months, depending upon the type of graft material used. Once the graft has matured, the implants can be placed.
The sinus graft makes it possible for many patients to have dental implants that previously had no other option besides wearing loose dentures.
A sinus augmentation is generally performed at Dr. Emami‘s office under local anesthesia. Some patients may request oral or intravenous sedative medication as well.
Nerve Repositioning
The inferior alveolar nerve, which gives feeling to the lower lip and chin, may need to be moved in order to make room for the placement of dental implants in the lower jaw. A nerve repositioning procedure is limited to the lower jaw and may be indicated when teeth are missing in the area of the two back molars and/or second premolars. This procedure is considered a very aggressive approach since there is almost always some postoperative numbness of the lower lip and jaw area, which typically dissipates very slowly, but may be permanent. Usually other, less aggressive options are considered first (placement of blade implants, etc).
Typically, we remove an outer section of the cheek on the side of the lower jaw bone in order to expose the nerve and vessel canal. We then isolate the nerve and vessel bundle in that area and slightly pull it out to the side. We then place the implants while tracking the neuro-vascular bundle. Then the bundle is released and placed back over the implants. The surgical access is refilled with bone graft material of the surgeon’s choice and the area is closed.
These procedures may be performed separately or together, depending upon the individual’s condition. As stated earlier, there are several areas of the body that are suitable for attaining bone grafts. In the maxillofacial region, bone grafts can be taken from inside the mouth, in the area of the chin or third molar region, or in the upper jaw behind the last tooth. In more extensive situations, a greater quantity of bone can be attained from the hip or the outer aspect of the tibia at the knee. When we use the patient’s own bone for repairs or additions, we generally get the best results.
In many cases, we can use allograft material to implement bone grafting for dental implants. This bone is prepared from cadavers and is used to get the patient’s own bone to grow into the repair site. It is quite effective and very safe. Synthetic materials can also be used to stimulate bone formation. We even use factors from your own blood to accelerate and promote bone formation in graft areas.
These surgeries are performed in the out-office surgical suite under IV sedation or general anesthesia. After discharge, bed rest is recommended for one day as well as limited physical activity for one week.
Socket Preservation
Preserving Your Jaw Bone after Extraction
Removal of teeth is sometimes necessary because of pain, infection, bone loss, or due to a fracture in the tooth. The bone that holds the tooth in place (the socket) is often damaged by disease and/or infection, resulting in a deformity of the jaw after the tooth is extracted. In addition, when teeth are extracted, the surrounding bone and gums can shrink and recede very quickly, resulting in unsightly defects and a collapse of the lips and cheeks.
These jaw defects can create major problems in performing restorative dentistry whether your treatment involves dental implants, bridges, or dentures. Jaw deformities from tooth removal can be prevented and repaired by a procedure called socket preservation. Socket preservation can greatly improve your smile’s appearance and increase your chances for successful dental implants.
Several techniques can be used to preserve the bone and minimize bone loss after an extraction. In one common method, the tooth is removed, and the socket is filled with bone or bone substitute. It is then covered with gum, artificial membrane, or tissue, which encourages your body’s natural ability to repair the socket. With this method, the socket heals, eliminating shrinkage and collapse of the surrounding gum and facial tissues. The newly formed bone in the socket also provides a foundation for an implant to replace the tooth. If your dentist has recommended tooth removal, be sure to ask if socket preservation is necessary. This is particularly important if you are planning on replacing the front teeth.
Wisdom Teeth
What are wisdom teeth?
Third molars are commonly referred to as wisdom teeth. They are usually the last teeth to develop and are located in the back of your mouth behind your second molars. Their development is usually completed between the middle teenage years and early 20s, a time traditionally associated with the onset of maturity and the attainment of wisdom.
Call (513) 232-4600 (Jager Court) or (513) 923-1500 (Banning Road) to schedule your wisdom teeth consultation.
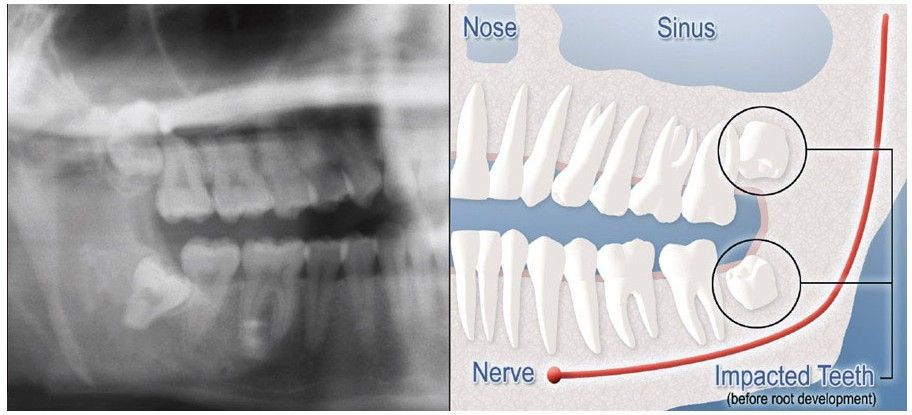
Impacted Wisdom Teeth
What is an impacted tooth?
Although most people develop and grow 32 permanent adult teeth, many times their jaws are too small to accommodate the four wisdom teeth. When inadequate space prevents the teeth from erupting, they are called impacted wisdom teeth. This indicates their inability to erupt into the proper position for chewing and cleaning.
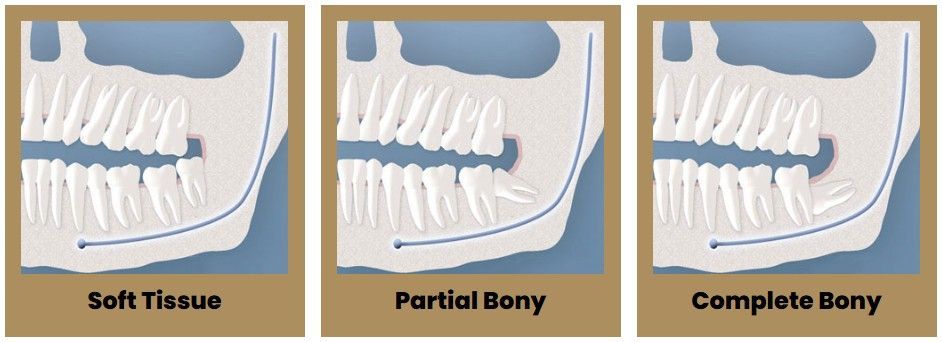
Types Of Impactions
We will need to see you for a consultation to determine if you will benefit from wisdom tooth removal. A special X-ray of your mouth and jaws (panorex) will be taken to determine if your wisdom teeth are impacted, if there is room for them to erupt, and how difficult it will be to have them removed.
- Soft Tissue Impaction: There is not enough room to allow the gum tissue to retract for adequate cleaning of the tooth.
- Partial Bony Impaction: There is enough space to allow the wisdom tooth to partially erupt. However, the tooth cannot function properly in the chewing process and creates cleaning problems, among others.
- Complete Bony Impaction: There is NO space for the tooth to erupt. It remains embedded in the jaw bone or if even partially visible requires complex surgical techniques for removal. The impacted wisdom tooth may also be in an unusual position and difficult to remove. This situation can also arise when the shape or size of the jaw bone and other facial structures make removal of this tooth significantly more complex.
Wisdom Teeth Removal
Oral Examination for Extraction of Wisdom Teeth
With an oral examination and X-rays of the mouth, Dr. Emami can evaluate the position of the wisdom teeth and predict if there are present or future potential problems. Studies have shown that early evaluation and treatment result in a superior outcome for the patient. Patients are generally first evaluated in the mid-teenage years by their dentist, orthodontist, or by an oral and maxillofacial surgeon.
All outpatient surgery is performed under appropriate anesthesia to maximize patient comfort. Our doctors are trained, licensed, and highly experienced in providing various types of anesthesia for patients.
Why should I have my wisdom teeth removed?
If you do not have enough room in your mouth for your third molars to fully erupt, a number of problems can happen. Impacted wisdom teeth should be removed before their root structure is fully developed. In some patients, it is as early as 12 or 13; and in others, it may not be until the early 20s. Problems tend to occur with increasing frequency after the age of 30. Some of the possible problems related to not removing your wisdom teeth include:
Infection:
The most frequent clinical problem we see is pericoronitis, (a localized gum infection). Without enough room for total eruption, the gum tissue around the wisdom tooth can become irritated and infected, resulting in recurrent pain, swelling, and problems with chewing and/or swallowing.
Cyst Formation:
Non-infectious diseases may also arise in association with an impacted wisdom tooth. Cysts are fluid-filled “balloons” inside the jaw bone that develop as a result of impacted teeth and slowly expand, destroying adjacent jaw bone and occasionally teeth. They can be very difficult to treat if your wisdom teeth are not removed in your teenage years. Although rare, tumors can be associated with the delayed removal of wisdom teeth.
Possible Crowding:
Impacted wisdom teeth may contribute to crowding of your teeth. This is most noticeable with the front teeth, primarily the lower front teeth, and is most commonly seen after a patient has had braces. There are a number of factors that cause teeth to crowd after braces or in early adulthood. Retained, impacted wisdom teeth may be a contributing factor. Unless you have an active problem when you see the oral surgeon, the reason for removal is primarily to prevent long-term damage to your teeth, gums, and jaw bone.
Damage to Adjacent Teeth:
If there is inadequate room to clean around the wisdom tooth, the tooth directly in front, the second molar, can be adversely affected resulting in gum disease, bone loss around the tooth, and/or decay.
What if I don’t have my wisdom teeth removed as a teenager or young adult?
As wisdom teeth develop, the roots become longer and the jaw bone more dense. When it is necessary to remove impacted wisdom teeth in your 30s, 40s, or beyond, the post-operative course can be prolonged, and there is a higher complication rate. Treating these complications is often more difficult and less predictable than with a younger patient. Healing may be slower and the chance of infection can be increased. If your impacted wisdom teeth are not removed in your teenage years or early in your 20s and are completely impacted in bone, it may be advisable to wait until a localized problem (such as cyst formation or localized gum disease and bone loss) develops. In general, you will heal faster, more predictably, and have fewer complications if treated in your teens or early 20s.
What happens on the day wisdom teeth are removed?
Most people prefer to be unaware of the experience when they have their wisdom teeth removed and usually decide to be sedated. You will be provided with appropriate anesthesia options at your consultation. All outpatient surgery is performed under appropriate anesthesia to maximize your comfort. Our office staff has the training, licensing, and experience to provide the various types of anesthesia.
These services are provided in an environment of optimum safety, utilizing modern monitoring equipment and a well-trained, experienced staff. The surgical care team, the office facilities, and the doctors are inspected on behalf of the Board of Dental Examiners on a regular basis.
On the day of your procedure, you will take medications to help minimize post-operative pain and swelling. We ask that a parent or responsible adult accompanies you to the office and plans to stay with you the rest of the day. The procedure will take about 30 to 60 minutes, and you will probably be in the office for 90 minutes. Recent advances in medicine and technology allow patients to undergo wisdom tooth removal in a manner that promotes rapid healing and minimal post-operative discomfort. State-of-the-art sterilization and infection control techniques are used at all times.
On the morning or afternoon of your surgery, it is essential that you have nothing to eat or drink (excluding prescription medications with a sip of water) for at least six hours (preferably longer). This does not mean you should try to fit in one “last meal” exactly six hours before your surgery. Having anything in your stomach can increase the risk for serious anesthetic complications, including nausea and vomiting. Your procedure will be rescheduled if you have not heeded these guidelines. We may provide you with a prescription for pain medication at your consultation appointment, which, for your convenience, can be filled in advance. When you are seated in the surgical room, we will make every effort to make you as comfortable as possible. If you are going to be sedated, we usually will place an IV in your left arm. This is a quick and nearly painless procedure that ensures optimal delivery of your medication. Local anesthesia is given to you afterward to ensure comfort and allow adequate time to travel home and rest. You will be sleepy for a significant portion of the day.
If your surgery requires stitches, these are usually the type that dissolve in three to five days and do not require removal. You may also notice a sensation of your gums feeling swollen and pulling away from your teeth. This is all part of the normal recovery, and it will subside in several days.
Once the local anesthesia wears off, you may require prescription pain medication. Please try non-narcotic anti-inflammatory medications such as ibuprofen (Advil®) first, to see if that adequately treats your pain. If not, begin your other prescription pain medication. The local anesthesia may last until the following day and should not be confused with an injury to your nerve. We recommend starting your post-operative diet with clear liquids such as Jello and broths, gradually increasing in substance as your body permits.
We do not recommend using dairy products, such as yogurt, ice cream or milkshakes, on the day of surgery as nausea and vomiting may develop in conjunction with the anesthetic and pain medication. If you are given antibiotics and you take birth control pills, please be aware that the birth control pills might become ineffective and take appropriate precautions.
What does wisdom tooth removal cost and is it covered by insurance?
The fee for your treatment is determined by a number of factors. These may include the difficulty involved in removing your teeth and which type of anesthesia is best for you. During your consultation appointment, the surgeon will need to review your X-rays, complete an examination, and determine the best option for anesthesia before an accurate estimate can be provided. Every insurance company has a different policy regarding the extent of coverage for a given surgical procedure. The oral surgeon’s office staff will help you obtain maximum insurance coverage for your treatment.
What if I have questions before surgery?
At the time of your consultation, your specific situation will be discussed in greater detail. We encourage you to ask any questions you may have. If new questions arise after your consultation, please call our office at (513) 232-4600 (Jager Court) or (513) 923-1500 (Banning Road) to speak to one of our patient care coordinators.
After Extraction of Wisdom Teeth
In most cases, the removal of wisdom teeth is performed under local anesthesia or general anesthesia. These options, as well as the surgical risks (i.e., sensory nerve damage, sinus complications), will be discussed with you before the procedure is performed. Once the teeth are removed, the gum is sutured. To help control bleeding, bite down on the gauze placed in your mouth. You will rest under our supervision in the office until you are ready to be taken home. If you have any questions, please do not hesitate to call us at Jager Court at (513) 232-4600 or at Banning Road at (513) 923-1500.
Our services are provided in an environment of optimum safety. We utilize modern monitoring equipment, and our staff is experienced in anesthesia techniques.
What will I feel like after wisdom teeth removal surgery?
On the first day after wisdom teeth removal surgery, you may experience some minor bleeding and pain. You should cover your pillowcase with something so that you don’t get any blood on it. Each individual’s reaction to surgery varies, and the sensation of pain can range from mild discomfort to severe pain. A variable amount of swelling can be expected following the surgery. This swelling usually peaks on the second day and should begin resolving on the third day. You can limit the amount of swelling you will have by using ice for the entire first day. The more ice you use the first day, the less swelling you are likely to have on the second day. Please remember to put ice on the first day, even if it is somewhat uncomfortable to have the cold next to your skin. On the third day, you will notice that your jaw muscles are stiff, and it is difficult to open your mouth normally. You can apply moist heat to your face on the second and third day, allowing your muscles to relax more and open wider. Most of the time, you will want to limit your activities for a few days. We ask that you follow your post-operative instructions closely. Doing so will make you as comfortable as possible during the first few days following your procedure. Please allow time for your body to begin healing before resuming an active social, academic, or athletic schedule. Most patients feel like they are over the hump and on their way to recovery in three to five days.
Are there any problems after the extraction of wisdom teeth?
As with any medical procedure, there can be complications or an unanticipated result. Some complications that patients undergoing wisdom tooth extraction may experience include:
- damage to the sensory nerve that supplies sensation to the lips and tongue
- sinus communication
- infections
- dry sockets
After the procedure, our assistants will review your post-operative instructions with your escort. We ask that you follow these instructions closely, as they will make you most comfortable following your procedure. If you were sedated, you will be comfortable and drowsy when you leave the office. Most patients prefer to go home and rest with no other physical or scholastic activities planned for a few days. With any medical procedure, there can be unexpected results. These can include delayed healing, infection and post-operative numbness or tingling in your lip, chin, or tongue. Dr. Emami will review relevant post-operative events with you and answer any questions during your office visit.
Damage to Sensory Nerve:
A primary concern is a nerve within the lower jaw bone that supplies feeling to the lower lip, chin, and tongue. This nerve is frequently very close to the roots of the lower wisdom teeth. Having these teeth out between the ages of 12 and 18 usually provides shorter roots so that the nerve is not so close to the roots of these teeth. Occasionally, when the teeth are removed, and especially in older patients, the nerve can become injured. When local anesthesia wears off, you may experience a tingling or numbing sensation in the lower lip, chin, or tongue. Should this occur, it is usually temporary and will resolve gradually over a period of weeks or months. On rare occasions, it can result in a permanent alteration of sensation similar to having local anesthesia. We feel that you should be aware of this possibility before consenting to surgery.
Sinus Communication:
The upper wisdom teeth are situated close to your sinuses, and their removal can result in an opening between your mouth and the sinus. Once again, if the teeth are removed at an early age, the root formation is minimal, and this complication is very unlikely. However, if it does occur, it will usually close spontaneously, but we may give you special instructions to follow, such as avoid blowing your nose for two or three days following the surgery. You can wipe your nose, but don’t blow your nose. If you have to sneeze, you should sneeze with an open mouth into a tissue. Pressure should not be created in the sinus area, which may dislodge the healing blood clot. If you sense this condition occurring after the surgery, please contact the office. An additional procedure may RARELY be necessary to close the opening.
Dry Sockets:
Dry sockets continue to be the most common problem people experience following dental surgery. They arise due to premature loss of a blood clot in the empty tooth socket. This seems to occur with greater frequency in people who smoke or are taking birth control pills. While both jaws can be affected, they usually occur in the lower jaw on the third to fifth day. They cause a deep, dull, continuous aching on the affected side(s). Patients may first notice the pain starting in the ear radiating down toward the chin.
The symptoms frequently begin in the middle of the night, and your pain medication regimen may not help. Treatment can involve changing your prescription. Occasionally it is helpful to place a medicated dressing in the empty tooth socket. This will help decrease the pain and protect the socket from food particles. The effectiveness in alleviating the pain lasts for 24-48 hours and may require dressing changes every day or two, for five to seven days. Dressings usually are removed when you have been pain-free for two to three days.
The dressing doesn’t aid in healing. The only reason to place a dressing is for pain control. If medication is controlling the pain, the socket will heal without a dressing. Following removal of the dressing, an irrigation device may be provided to help you to keep food particles from lodging in the extraction site.
Infection:
Occasionally, post-operative infections occur. This usually requires an office visit and clinical examination. Many times, just placing you on an antibiotic for one week will take care of the infection. If it persists, the area will have to be drained and cleaned. Other temporary problems you may experience in the post-operative period include stiffness of the jaws, chafing around the corners of your lips, facial bruising, and blood oozing from the extraction sites. The post-operative instruction sheet we will provide should answer many of the questions related to these more common concerns. If not, don’t hesitate to call the office at (513) 232-4600 (Jager Court) or (513) 923-1500 (Banning Road).
Orthognathic Surgery
Corrective Jaw Surgery
Orthognathic surgery is needed when the top and bottom jaws don’t meet correctly and/or teeth don’t adequately fit within the jaw. Teeth are straightened with orthodontics, and corrective jaw surgery repositions a misaligned jaw. This not only improves facial appearance but also ensures that teeth meet correctly and function properly.
Who needs orthognathic surgery?
People who can benefit from orthognathic surgery include those with an improper bite or jaws that are positioned incorrectly. Jaw growth is a gradual process; and in some instances, the upper and lower jaws may grow at different rates. The result can be a host of problems that may affect chewing function, speech, or long-term oral health and appearance. Injury to the jaw and birth defects can also affect jaw alignment. Orthodontics alone can correct bite problems when only the teeth are involved. Orthognathic surgery may be required for the jaws when repositioning is necessary.
Difficulty in the following areas should be evaluated:
- Difficulty in chewing, biting, or swallowing
- Speech problems
- Chronic jaw or TMJ pain
- Open bite
- Protruding jaw
- Breathing problems
Any of these symptoms can exist at birth, be acquired after birth as a result of hereditary or environmental influences, or as a result of trauma to the face. Before any treatment begins, a consultation will be held to perform a complete examination with X-rays. During the pre-treatment consultation process, feel free to ask any questions that you have regarding your treatment. When you are fully informed about the aspects of your care, you and your dental team can make the decision to proceed with treatment together.
Technology & Orthognathic Surgery
Dr. Emami uses modern computer-aided techniques and three-dimensional models to show you exactly how your surgery will be approached. Using comprehensive facial X-rays and computer video imaging, we can show you how your bite will be improved and even give you an idea of how you’ll look after surgery. This helps you understand the surgical process and the extent of the proposed treatment.
If you are a candidate for corrective jaw surgery, Dr. Emami will work closely with your dentist and orthodontist during your treatment. The actual surgery can move your teeth and jaws into a new position that results in a more attractive, functional, and healthy dental-facial relationship.
What to Expect
- Corrective jaw surgery is a significant intervention requiring many months of preparation.
- The surgery is performed in the hospital and can last between one to four hours.
- Hospital stays of one to three days are normal.
- Braces are maintained during surgery and may need to be removed six to 12 months after surgery.
- The greatest impact of orthognathic surgery is the recovery phase.
- Patients typically may be off work/school from two weeks to one month after surgery.
- Return to normal chewing function may take two months, and full function may take one year.
- Our goal is to ensure that you are well taken care of during and after surgery.
- Weekly appointments are required for up to two months after surgery.
Facial Trauma
Orthognathic surgery is needed when the top and bottom jaws don’t meet correctly and/or teeth don’t adequately fit within the jaw. Teeth are straightened with orthodontics, and corrective jaw surgery repositions a misaligned jaw. This not only improves facial appearance but also ensures that teeth meet correctly and function properly.
Dr. Emami meets and exceeds these modern standards. He is trained, skilled, and uniquely qualified to manage and treat facial trauma. Dr. Emami is on staff at local hospitals and deliver emergency room coverage for facial injuries, which include the following conditions:
- Facial lacerations
- Intraoral lacerations
- Avulsed (knocked out) teeth
- Fractured facial bones (cheek, nose, or eye socket)
- Fractured jaws (upper and lower jaw)
The Nature of Maxillofacial Trauma
There are a number of possible causes of facial trauma, such as motor vehicle accidents, accidental falls, sports injuries, interpersonal violence, and work-related injuries. Types of facial injuries can range from injuries to teeth to extremely severe injuries to the skin and bones of the face. Typically, facial injuries are classified as either soft tissue injuries (skin and gums), bone injuries (fractures), or injuries to special regions (such as the eyes, facial nerves, or the salivary glands).
Soft Tissue Injuries of the Maxillofacial Region
When soft tissue injuries, such as lacerations, occur on the face they are repaired by suturing. In addition to the obvious concern of providing a repair that yields the best cosmetic result possible, care is taken to inspect for and treat injuries to structures such as facial nerves, salivary glands, and salivary ducts (or outflow channels). Dr. Emami is a well-trained oral and maxillofacial surgeon and is proficient at diagnosing and treating all types of facial lacerations.
Bone Injuries of the Maxillofacial Region
Fractures to the bones in the face are treated in a similar manner to fractures in other parts of the body. The specific form of treatment is determined by various factors, which include the location of the fracture, the severity of the fracture, and the age and general health of the patient. When an arm or leg is fractured, a cast is often applied to stabilize the bone to allow for proper healing. Since a cast cannot be placed on the face, other means have been developed to stabilize facial fractures.
One of these options involves wiring the jaws together for certain fractures of the upper and/or lower jaw. Certain other types of fractures of the jaw are best treated and stabilized by the surgical placement of small plates and screws at the involved site. This technique of treatment can often allow for healing and eliminates the necessity of having the jaws wired together. This technique is called “rigid fixation” of a fracture. The relatively recent development and use of rigid fixation has profoundly improved the recovery period for many patients, allowing them to return to normal function more quickly.
The treatment of facial fractures should be accomplished in a thorough and predictable manner. More importantly, the patient’s facial appearance should be minimally affected. An attempt at accessing the facial bones through the fewest incisions necessary is always made. At the same time, the incisions that become necessary are designed to be small and, whenever possible, are placed so that the resultant scar is hidden.
Injuries to the Teeth & Surrounding Dental Structures
Isolated injuries to teeth are quite common and may require the expertise of various dental specialists. Oral surgeons usually are involved in treating fractures in the supporting bone, or in replanting teeth that have been displaced or knocked out. These types of injuries are treated by one of a number of forms of splinting (stabilizing by wiring or bonding teeth together). If a tooth is knocked out, it should be placed in salt water or milk. The sooner the tooth is re-inserted into the dental socket, the better chance it will survive. Therefore, the patient should see a dentist or oral surgeon as soon as possible. Never attempt to wipe the tooth off, since remnants of the ligament that hold the tooth in the jaw are attached and are vital to the success of replanting the tooth. Other dental specialists may be called upon, such as endodontists, who may be asked to perform root canal therapy, and/or restorative dentists, who may need to repair or rebuild fractured teeth. In the event that injured teeth cannot be saved or repaired, dental implants are often now utilized as replacements for missing teeth.
The proper treatment of facial injuries is now the realm of specialists who are well-versed in emergency care, acute treatment, long-term reconstruction, and rehabilitation of the patient.
Tooth Extractions
You and Dr. Emami may determine that you need a tooth extraction for any number of reasons. Some teeth are extracted because they are severely decayed; others may have advanced periodontal disease or have broken in a way that cannot be repaired. Other teeth may need removal because they are poorly positioned in the mouth (such as impacted teeth) or in preparation for orthodontic treatment.
The removal of a single tooth can lead to problems related to your chewing ability, problems with your jaw joint, and shifting teeth, which can have a major impact on your dental health.
To avoid these complications, in most cases, Dr. Emami will discuss alternatives to extractions as well as replacement of the extracted tooth.
The Tooth Extraction Process
At the time of extraction, the doctor will need to numb your tooth, jaw bone, and gums that surround the area with a local anesthetic.
During the extraction process, you will feel a lot of pressure. This is from the process of firmly rocking the tooth in order to widen the socket for removal. You feel the pressure without pain as the anesthetic has numbed the nerves stopping the transference of pain, yet the nerves that transmit pressure are not profoundly affected.
If you do feel pain at any time during the extraction, please let us know right away.
Sectioning a Tooth
Some teeth require sectioning. This is a very common procedure done when a tooth is so firmly anchored in its socket or the root is curved and the socket can’t expand enough to remove it. The doctor simply cuts the tooth into sections then removes each section one at a time.
After Tooth Extraction
For details on home care after tooth extraction, click here.
Pre-Prosthetic Surgery
The preparation of your mouth before the placement of a prosthesis is referred to as pre-prosthetic surgery.
Some patients require minor oral surgical procedures before receiving a partial or complete denture in order to ensure the maximum level of comfort. A denture sits on the bone ridge, so it is very important that the bone is the proper shape and size. If a tooth needs to be extracted, the underlying bone might be sharp and uneven. For the best fit of a denture, the bone might need to be smoothed or reshaped. Occasionally, excess bone may need to be removed prior to denture insertion.
One or more of the following procedures might need to be performed in order to prepare your mouth for a denture:
- Bone smoothing and reshaping
- Removal of excess bone
- Bone ridge reduction
- Removal of excess gum tissue
- Exposure of impacted teeth
We will review your particular needs with you during your appointment.
Oral Pathology
The inside of the mouth is normally lined with a special type of skin (mucosa) that is smooth and coral pink in color. Any alteration in this appearance could be a warning sign for a pathological process. The most serious of these is oral cancer.
The following can be signs at the beginning of a pathological process or cancerous growth:
- Reddish patches (erythroplasia) or whitish patches (leukoplakia) in the mouth
- A sore that fails to heal and bleeds easily
- A lump or thickening on the skin lining the inside of the mouth
- Chronic sore throat or hoarseness and/or difficulty in chewing or swallowing
These changes can be detected on the lips, cheeks, palate, and gum tissue around the teeth, tongue, face, and/or neck. Pain does not always occur with pathology, and curiously, is not often associated with oral cancer. However, any patient with facial and/or oral pain without an obvious cause or reason may also be at risk for oral cancer.
We would recommend performing an oral cancer self-examination monthly. Remember that your mouth is one of your body’s most important warning systems. Do not ignore suspicious lumps or sores. Please contact us so that we can assist you with any questions or concerns.
Exposure of Impacted Teeth
What is an impacted tooth?
An impacted tooth simply means that it is “stuck” and cannot erupt into function. Patients frequently develop problems with impacted third molar (wisdom) teeth. These teeth get “stuck” in the back of the jaw and can develop painful infections, among a host of other problems (see Wisdom Teeth under Procedures). Since there is rarely a functional need for wisdom teeth, they are usually extracted if they develop problems. The maxillary cuspid (upper eyetooth) is the second most common tooth to become impacted. The cuspid tooth is a critical tooth and plays an important role in your “bite.” The cuspid teeth are very strong biting teeth and have the longest roots of any human teeth. They are designed to be the first teeth that touch when your jaws close together so that they guide the rest of the teeth into the proper bite.
Normally, the maxillary cuspid teeth are the last of the “front” teeth to erupt into place. They usually come into place around age 13 and cause any space left between the upper front teeth to close tighter together. If a cuspid tooth gets impacted, every effort is made to get it to erupt into its proper position. The techniques involved to aid eruption can be applied to any impacted tooth in the upper or lower jaw, but most commonly they are applied to the maxillary cuspid (upper eye) teeth. As many as 60 percent of these impacted eyeteeth are located on the palatal (roof of the mouth) side of the dental arch. The remaining impacted eye teeth are found in the middle of the supporting bone but are stuck in an elevated position above the roots of the adjacent teeth or are out to the facial side of the dental arch.
Early Recognition of Impacted Eyeteeth Is the Key to Successful Treatment
The older the patient, the more likely an impacted eyetooth will not erupt by natural forces alone, even if the space is available for the tooth to fit in the dental arch. A panoramic X-ray, along with a dental examination, will help determine whether all the adult teeth are present or if some adult teeth are missing.
Treatment may require referral to an oral surgeon for extraction of over-retained baby teeth and/or selected adult teeth that are blocking the eruption of the all-important eyeteeth. The oral surgeon will also need to remove any extra teeth (supernumerary teeth) or growths that are blocking the eruption of any adult teeth.
Impacted tooth success by patient’s age:
- 11-12 years old – with space opened for eruption, good chance for success.
- 13-14 years old – the impacted eyetooth will not erupt by itself, even with the space cleared for its eruption.
- Over 40 years old – much higher chance that the tooth will be fused in position. The only option is to extract the impacted tooth and replace it with a crown on a dental implant or a fixed bridge.
What happens if the eyetooth will not erupt when proper space is available?
In cases where the eyeteeth will not erupt spontaneously, the orthodontist and oral surgeon will work together to get these teeth to erupt. Each case must be evaluated on an individual basis, but treatment will usually involve a combined effort between the orthodontist and the oral surgeon. The oral surgeon will expose and bracket the impacted eyetooth.
The goal is to erupt the impacted tooth and not to extract it. Once the tooth has moved into its final position, the gum around it will be evaluated. In some circumstances, there may be some minor “gum surgery” required.
What to expect from surgery to expose & bracket an impacted tooth
The surgery to expose and bracket an impacted tooth is a very straightforward surgical procedure that is performed in the oral surgeon’s office. For most patients, it is performed using laughing gas and local anesthesia. In selected cases, it will be performed under IV sedation if the patient desires to be asleep, but this is generally not necessary for this procedure. If the procedure only requires exposing the tooth with no bracketing, the time required will be shortened by about one-half. These issues will be discussed in detail at your preoperative consultation with your doctor.
Refer to Preoperative Instructions under Surgical Instructions on this website for a review of any details. Simply call Oral & Maxillofacial Surgery of Ohio at (513) 232-4600 (Jager Court) or (513) 923-1500 (Banning Road) if you have any questions.
3D Imaging
Cone Beam CT Scan
The CS 9300 system gives our oral and maxillofacial practice state-of-the-art technology to help Dr. Emami diagnose potential issues more accurately and provide treatment with unprecedented confidence. Unlike a traditional spiral CT scanner, this 3D system utilizes cone beam CT technology and provides precise, crystal-clear digital images while minimizing your exposure to radiation.
Our new 3D system enables us to perform a wider range of diagnoses and treatments in our office, helping to reduce multiple visits. The CS 9300 scanner allows us to choose the field of view, or scanning area, that best suits your specific treatment needs. This helps to limit your radiation exposure because we are focusing specifically on your area of concern.
The CS 9300 system brings the latest 3D technology to Oral & Maxillofacial Surgery of Ohio, providing unmatched visualization of anatomical detail, which aids in treatment planning and helps us to better explain the particulars of your case as well as address any questions you may have. Dr. Emami can use this innovative technology to quickly and easily share 3D images of the area of concern with your referring doctor – allowing the doctors to collaborate on your care, improving your experience, and delivering a positive treatment outcome.
Anesthesia
Several methods of anesthesia are available. The method of anesthesia that is chosen for or by a patient depends upon the nature of the surgical procedure and the patient’s level of apprehension.
Anesthesia Options
Local Anesthetic
Description: The patient remains totally conscious throughout the procedure. A local anesthetic (e.g. lidocaine) is administered in the area where the surgery is to be performed. Local anesthetic is used in conjunction with the other methods of anesthesia in all oral surgery procedures.
Usual Indications: Simple oral surgery procedures such as minor soft tissue procedures and simple tooth extractions.
Nitrous Oxide Sedation with Local Anesthetic
Description: A mixture of nitrous oxide (laughing gas) and oxygen is administered through a nasal breathing apparatus. The patient remains conscious in a relaxed condition. Nitrous oxide has a sedative and analgesic (pain- controlling) effect.
Usual Indications: Simple oral surgery procedures to more involved procedures, such as removal of wisdom teeth and placement of dental implants.
Office Based General Anesthesia with Local Anesthetic*
Description: Medications are administered through an intravenous line (I.V.). The patient falls asleep and is completely unaware of the procedure being performed. Medications most commonly used are Fentanyl (opiate), Versed (benzodiazepine), Ketamine, and Diprivan. Supplemental oxygen is delivered through a nasal breathing apparatus, and the patient’s vital signs are closely monitored.
Usual Indications: General anesthesia is available for all types of oral surgery. A patient may choose general anesthesia for simple procedures, depending on their level of anxiety. Most people having their wisdom teeth removed or having a dental implant placed will choose general anesthesia. General anesthesia may be necessary if local anesthesia fails to anesthetize the surgical site, which often occurs in the presence of infection.
Hospital or Surgery Center Based General Anesthesia
Description: A patient is admitted to a hospital or surgery center where anesthesia is administered by an anesthesiologist.
Usual Indications: Indicated for patients undergoing extensive procedures such as face and jaw reconstruction and TMJ surgery. Also indicated for patients with medical conditions such as heart disease or lung disease who require general anesthesia.
To administer general anesthesia in the office, an oral surgeon must have completed at least three months of hospital-based anesthesia training. Qualified applicants will then undergo an in-office evaluation by a state dental board appointed examiner. The examiner observes an actual surgical procedure during which general anesthesia is administered to the patient. The examiner also inspects all monitoring devices and emergency equipment and tests the doctor and the surgical staff on anesthesia-related emergencies. If the examiner reports successful completion of the evaluation process, the state dental board will issue the doctor a license to perform general anesthesia. The license is renewable every two years if the doctor maintains the required amount of continuing education units related to anesthesia.
Again, when it comes to anesthesia, our first priority is the patient’s comfort and safety. If you have any concerns regarding the type of anesthesia that will be administered during your oral surgery procedure, please do not hesitate to discuss your concerns with your doctor at the time of your consultation.
Intravenous Sedation (“Twilight Sedation”)
Our office offers our patients the option of intravenous sedation or dental intravenous anesthesia; or to some, it is referred to as “Twilight Sedation” for their dental treatment. Intravenous sedation or “twilight sleep” helps you to be comfortable and calm when undergoing dental procedures. Your treatment can be completed under intravenous sedation. Intravenous sedation or “IV sedation” (twilight sedation) is designed to better enable you to undergo your dental procedures while you are very relaxed; it will enable you to tolerate as well as not remember those procedures that may be very uncomfortable for you. IV sedation will essentially help alleviate the anxiety associated with your treatment. You may not always be asleep but you will be comfortable, calm and relaxed, drifting in and out of sleep—a “twilight sleep.”
If you choose the option of intravenous sedation, your IV sedation/anesthesia is administered and monitored by the doctor, therefore eliminating the costly expense of having your treatment carried out in an operating room or same- day surgical facility.
How is the IV sedation administered?
A thin needle will be introduced into a vein in your arm or hand. The needle will be attached to an intravenous tube through which medication will be given to help you relax and feel comfortable. At times, a patient’s vein may not be maintainable; in these situations, the medications will be administered and the needle retrieved—both scenarios will achieve the same desired level of conscious sedation. Once again, some patients may be asleep while others will slip in and out of sleep. Some patients with medical conditions and/or on specific drug regimens may only be lightly sedated and may not sleep at all.
The goal of IV sedation is to use as little medication as possible to get the treatment completed. It is very safe—much safer than oral sedation. With IV sedation, a constant “drip” is maintained via the intravenous tube. At any time, an antidote can be administered to reverse the effects of the medications if necessary. Along with IV sedation, there are also other different “levels” of sedation available to you in our office. There is nitrous oxide analgesia.
Nitrous Oxide (Laughing Gas)
Nitrous oxide is a sweet-smelling, non-irritating, colorless gas that you can breathe. Nitrous oxide has been the primary means of sedation in dentistry for many years. Nitrous oxide is safe; the patient receives 50-70% oxygen with no less than 30% nitrous oxide. Patients are able to breathe on their own and remain in control of all bodily functions. The patient may experience mild amnesia and may fall asleep, not remembering all of what happened during their appointment.
There are many advantages to using Nitrous Oxide:
- The depth of sedation can be altered at any time to increase or decrease sedation.
- There is no after-effect such as a “hangover.”
- Inhalation sedation is safe with no side effects on your heart and lungs, etc.
- Inhalation sedation is very effective in minimizing gagging.
- It works rapidly as it reaches the brain within 20 seconds. In as few as two to three minutes, its relaxation and pain-killing properties develop.
Reasons to Not use Nitrous Oxide
Though there are no major contraindications to using nitrous oxide, you may not want to use it if you have emphysema, exotic chest problems, M.S., a cold, or other difficulties with breathing. You may want to ask your dentist for a “five-minute trial” to see how you feel with this type of sedation method before proceeding.
Reviews

Two Locations to Serve You
Oral & Maxillofacial Surgery of Ohio offers two convenient locations in Cincinnati.
Request Appointment Today!
Why Choose Us for Your Oral Surgery Needs
When it comes to oral surgery, you deserve a provider who prioritizes your comfort and care. Here’s what sets Oral & Maxillofacial Surgery of Ohio apart:
- Welcoming environment for all oral procedures
- State-of-the-art equipment
- Low-stress setting
- Committed to excellence in patient care
Don’t wait to address your oral health needs. Contact us now to schedule your consultation and experience the difference our expert care can make.
Contact Us
Ready to improve your oral health with our specialized surgical procedures?
Get in touch with Oral & Maxillofacial Surgery of Ohio in Cincinnati today. Our dedicated team is here to assist you with any questions and to schedule your appointment. Your optimal oral health is just a call away.
